Although the arrival of spring is usually synonymous with a rise in temperature or the blooming of plants, for many it can turn into a real nightmare, as it means the onset of spring allergies caused by pollen.
During spring there is also an increase in the emergence of certain pests such as the Processionary Caterpillar, an insect that invades arboreal species. With the arrival of good weather, its presence can cause eye risks, since it is wrapped in a series of tiny hairs that, when dispersed and floating in the air, can come into contact with our body and cause irritation to the skin, nose and eyes.
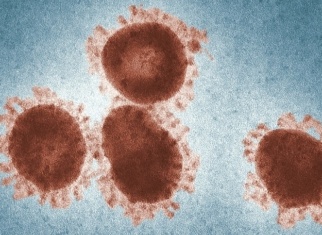
Sometimes the symptoms of spring allergies can be confused with the symptoms of other pathologies, such as dry eye or COVID-19. In some cases, both diseases can even coexist. Here we explain their similarities and differences.
What is ocular allergy?
Allergy is a self-defense response of the immune system to the presence of an allergen. Specifically, ocular allergy or allergic conjunctivitis is a common condition that usually affects the conjunctiva of the eye. The conjunctiva is a thin transparent mucous membrane (the white of the eye) that lines the anterior surface of the eyeball and posterior surface of the eyelids. It is the most immunologically active tissue of the eye, acting as a defense against infection and trauma. The conjunctiva, which helps hold both the eyelids and the eyeball together, is composed of the same sensitive tissue as the inner lining of the nose.
Conjunctivitis is characterized by recurrent and bilateral ocular inflammation caused by certain allergens, i.e. substances that, upon contact with ocular tissues, induce a state of hypersensitivity to this substance. Ocular allergies can be seasonal (especially in spring) or perennial (throughout the year).
What are its symptoms?
The most common ocular symptoms in eye allergy are:
- Redness
- Tearing
- Stinging
- Prickling
- Itching
- Eye swelling
How can I distinguish ocular allergy from coronavirus?
Some patients with coronavirus develop red eye or conjunctivitis, symptoms in common with ocular allergy. However, one of the main differences between allergy and COVID-19 is the occurrence of fever. Those with ocular allergy do not have fever as a symptom, unlike coronavirus patients who do. Other coronavirus symptoms not found in spring allergies include:
- Loss of smell and taste
- Diarrhea
- Nausea
- Cough
- Difficulty breathing
- Chest pain and pressure
- Excessive tiredness
In addition, allergic conjunctivitis occurs at the same time each year and may be accompanied by a runny nose and sneezing. However, conjunctivitis caused by a virus is usually an isolated incident and is accompanied by secretion that is stickier than tears.
Ocular allergy and dry eye
Dry eye or dry eye syndrome is a common eye disorder that occurs when there is a lack of lubrication and moisture on the surface of the eye. This occurs because the eye does not produce the necessary amount of tears to maintain good hydration and lubrication, or the tears are of poor quality.
Its symptoms can be similar to those of ocular allergies, so there are many patients who go to the doctor thinking they have a dry eye or ocular allergy, but in some cases the symptoms come from an association of causes.
Pollution in large cities associated with the pollen that appears with the seasonal change when spring arrives can cause problems in the eyes and respiratory tract in some people, who may experience an inflammatory reaction that irritates mucous membranes, such as the conjunctiva.

This state of eye inflammation can lead to decompensation of other conditions, such as dry eye. In cases of people already suffering from dry eye, their condition may worsen during the spring. They may experience discomfort when blinking and even watering of the eyes, which leads to confusion in the case of people who usually suffer from dry eyes.
In patients with dry eye, pollution and pollen particles can provoke an inflammatory effect that adds to the inflammatory effect that the person was already suffering due to the dryness of the eye.
The best way to prevent this imbalance is to protect the eyes and use artificial tears or eye drops to lubricate and clean the ocular surface.
Tips to reduce allergy symptoms
Allergic conjunctivitis is caused by the body’s reaction to the presence of an allergen. For this reason, it is important to follow these tips to minimize the chances of contact between the external agent and the eye:
- Wear glasses or sunglasses whenever possible to avoid contact with pollen.
- Close car and house windows to keep out foreign substances.
- Take off your jacket, shoes and cap when entering the house.
- Do not hang your clothes outside.
- Take a shower before going to bed to remove possible pollen from your body.
- Get information about the amount of pollen outside through meteorological channels. If the amount is very high, avoid going outdoors.

Pharmacological treatment to combat allergy
When dealing with a possible allergy, it is essential to know first the agent causing the allergy, in order to attack it or avoid contact with it. Although for some people this is obvious, there are many people who do not take it into account and go directly to a pharmacological treatment. Thus, if the cause is not avoided or reversed, the effect of the drugs will not solve the problem.
Once the cause has been detected, there are different treatments to alleviate the symptoms. It is important to consult with the ophthalmologist which is the most suitable drug for your case:
- Vasoconstrictors: reduce ocular reddening and eyelid edema by causing vasoconstriction of blood vessels.
- Anti-allergic and antihistamines: they inhibit mast cell degranulation and block histamine receptors.
- Nonsteroidal anti-inflammatory drugs: their effect is anti-inflammatory, analgesic and antipruritic.
- Corticosteroids: their action is only anti-inflammatory, but they are the most potent drugs. They should be used as a last resort because they may increase intraocular pressure or induce cataract formation.
In addition, it is advisable to visit the ophthalmologist during the spring season in cases of symptomatic dry eye or those that tend to have allergic reactions in order to take the necessary measures to avoid a decompensation that aggravates the discomfort.
More information:
- Villani E, Rabbiolo G, Nucci P. Ocular allergy as a risk factor for dry eye in adults and children. Curr Opin Allergy Clin Immunol. 2018
- Dupuis P, Prokopich CL, Hynes A, Kim H. A contemporary look at allergic conjunctivitis. Allergy Asthma Clin Immunol. 2020
- Is it COVID-19 or allergies? American Academy of Ophthalmology





Do you have any questions?
Contact us or request an appointment with one of our specialists.