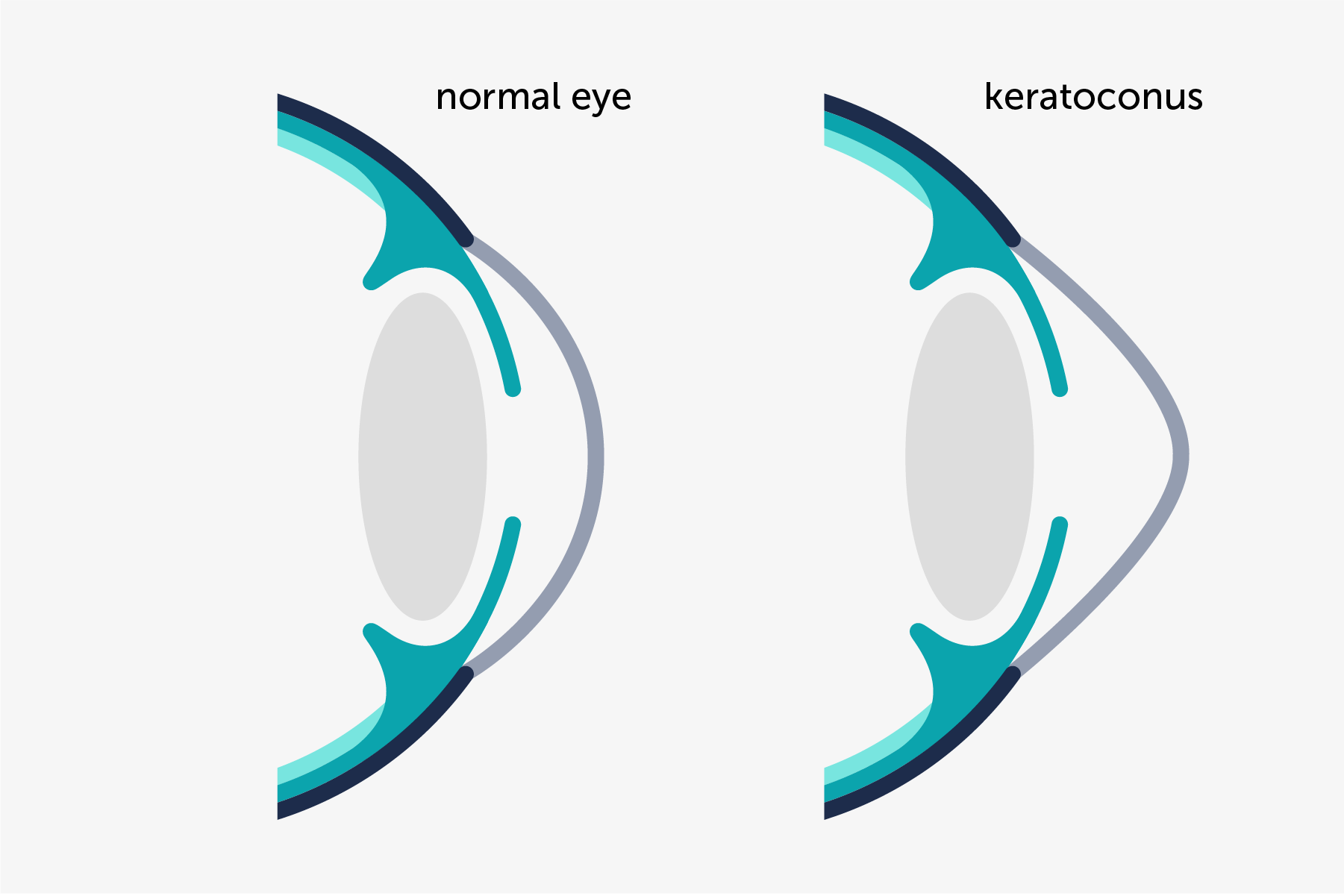
Keratoconus appears when the corneal tissue deteriorates, modifying its usual spherical shape by a cone shape. As the shape of the cornea is altered, the vision becomes distorted.
The cornea is one of the most important parts of the eye. Light enters the eye through the cornea and it focuses the light rays so that we can see clearly.
Keratoconus is one of the most common disorders of degenerative coranel diseases, it is usually detected during adolescence and can continue to develop into adulthood.
This ocular disorder is associated with a genetic basis, since 10% of those affected by this pathology have a relative who also has it. However it can also appear spontaneously.
Moreover, this visual disorder can be associated with other factors:
Keratoconus can develop in one of the two eyes, although it usually develops bilaterally.
The symptoms that usually appear are:
This disorder may progress for a period of 10 to 20 years during which the symptoms evolve.
Keratoconus can be diagnosed by performing a regular ophthalmological control.
Although the ophthalmologist has specific complementary tests that allow a more accurate diagnosis:
The treatment for keratoconus is established depending on the symptoms and the degree of evolution in which it is diagnosed.
As of today, the treatment serves to stop the development of this disorder, but there is no total cure.
The different types of treatment are:
There are no specific prevention measures to prevent this ocular disorder.
Ophthalmic controls on a regular basis are recommended since early detection is important for the approach of this disorder, especially in young patients, since it is the population with the highest risk.
It is recommended that those people who have a family history of this disease, go to check-ups often to make a good control of their eye health, as it is an almost asymptomatic pathology and, therefore, difficult to detect without ophthalmological control.
Contact us or request an appointment with our medical team.