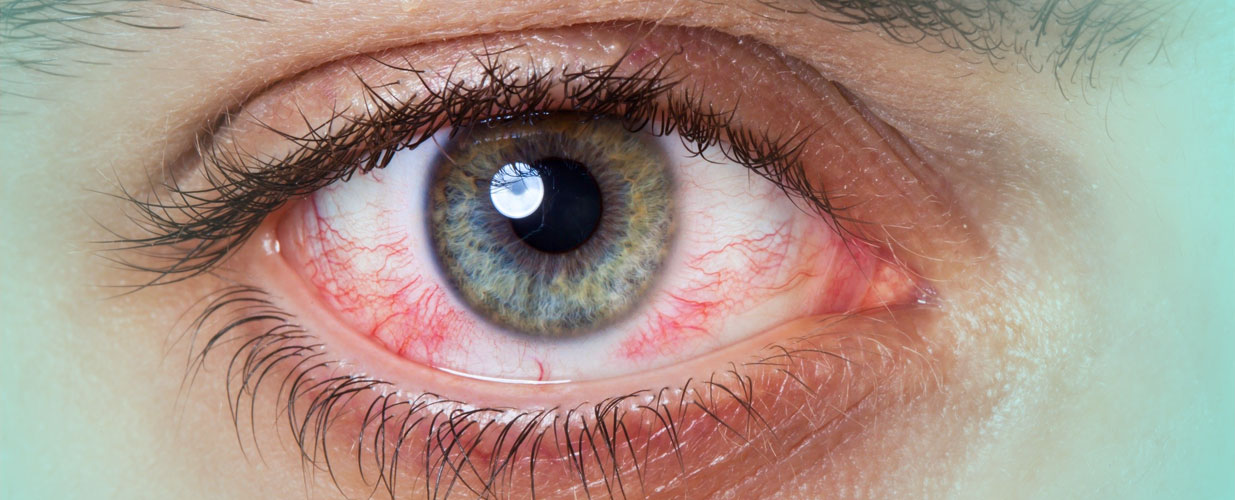
Conjunctivitis is an inflammation of the conjunctiva, which is the mucous membrane that covers the inside of the eyelids. It normally affects both eyes at the same time, although it can sometimes begin in one eye and then transfer to the other after a day or two. The condition in such cases is asymmetrical and more severe in the first eye. Conjunctivitis caused by an infectious agent (bacterial or viral) is normally acute. There are several causes and it is a very common condition that is not generally severe, although it can be very unpleasant.
Viral conjunctivitis is the most frequent cause of infectious conjunctivitis. It is often connected to colds and the most frequent cause is viruses of the adenovirus group. This type of conjunctivitis is very contagious, and can quickly spread from person to person and even cause epidemics. It is transmitted directly via contaminated hands or the use of contaminated objects (towels, pillows, toys, etc.).
With this type of conjunctivitis, the infection is caused by bacteria. These microorganisms can originate in the skin of the patient, the upper respiratory tract, or be transmitted by another person who has conjunctivitis. In some rare cases, conjunctivitis is caused by very aggressive germs, such as pseudomona aeruginosa in lens containers, C. diphtheria in children between 1 and 4.
Viral conjunctivitis
Bacterial conjunctivitis
This affects both eyes equally. The symptoms are usually less severe, provided there are no complications, and include:
Conjunctivitis is diagnosed through a clinical evaluation carried out by the ophthalmologist. If it is suspected then there is a specific test to look for the adenovirus in the conjunctiva called ADENO PLUS. A sample of conjunctival discharge is taken for cultivation in the lab in cases of severe bacterial conjunctivitis or with an unusual development.
Viral conjunctivitis
Bacterial conjunctivitis
In serious cases or those resistant to treatment, or if there is a deterioration in vision, you should contact your doctor again, even if you are following the correct treatment.
The vast majority of conjunctivitis improve spontaneously after a few weeks. Even with treatment, there can be a worsening in the first days and the other eye can be affected. Treatment does not shorten the duration of viral conjunctivitis. Viral conjunctivitis follows a clinical development (normally between 2 and 4 weeks) and medication can help to reduce symptoms, but it does not reduce the time needed to resolve the symptoms.
As a result, for a couple of months you may experience a foreign body sensation (like sand in your eye) or occasional reddening. With time this normally disappears. In these cases you are advised to use artificial tears and evaluate how it evolves. In the most complicated cases, between weeks 3 and 4 small marks may appear on the cornea that can reduce vision. This complication lasts longer than the others, for a few months, and can leave other marks and scars on the cornea, meaning that occasional tests are required until the symptoms are solved.
Contact us or request an appointment with our medical team.