
Macular epiretinal membrane causes a slow and progressive visual loss lasting months or years, and affecting one or both eyes. Generally, it causes image distortion, and undulation of straight lines. Numbers and letters can appear to be in another line, and perception of colors may be decreased.
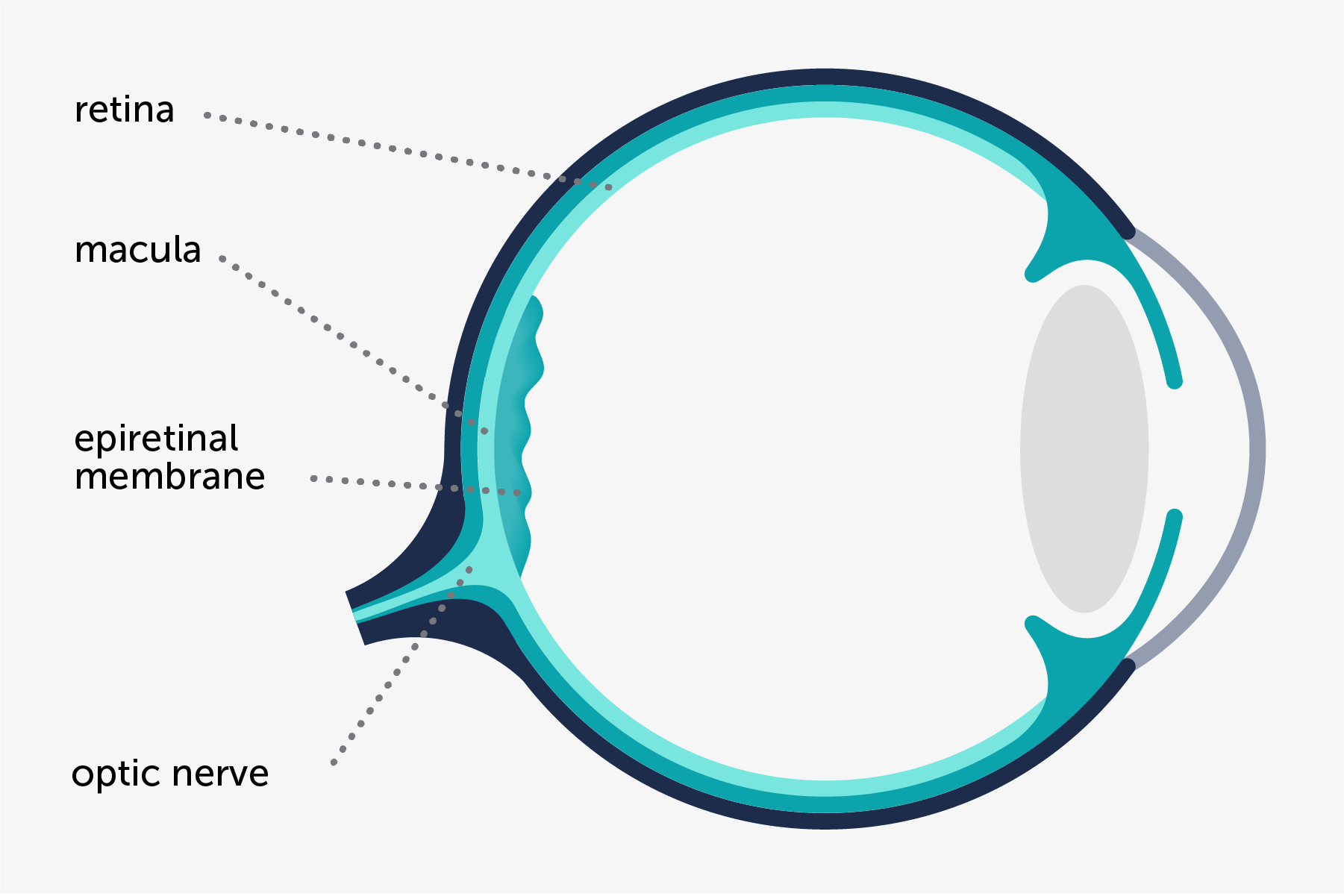
The typical sign is a semitransparent membrane that covers the rear surface of the retina, known as macula, which is the area responsible for detailed vision necessary to read. This membrane obscures and creases the retina in a greater or lesser degree, depending on its thickness and its capacity to contract.
In some cases, retinal cysts are detected, as a result of the leakage of fluid from blood vessels, which are subject to the membrane’s pulling effect. This disturbance is known as cystoid macular edema and implies a higher visual loss.
It appears in healthy patients without any evidence of other intraocular diseases.
First of all, it’s important to determine whether any of the abovementioned causes are responsible for the macular epiretinal membrane. If so, the first thing to do is to treat the underlying disease.
In idiopathic epiretinal membranes and, once resolved, in secondary epiretinal membranes, it is necessary to evaluate whether its removal can improve the visual acuity of the patient and reduce the vision distortion.
Before removing the epiretinal membrane, it is necessary to assess the patient’s degree of cataract. In patients who have cataracts, a combined surgical procedure consisting in the removal of the cataract and epiretinal membrane surgery is recommended, so as to avoid the need of a second intervention.
Personal history: drugs, systemic diseases, injuries, and eye diseases.
Full eye examination has to include:
Extraction of macular epiretinal membrane is performed in order to:
Cataract extraction is performed to:
Cataract extraction allows us to correct any refractive errors that the patient may have.
Patients who do not require surgery should undergo an examination every 6 months and should carry out self-monitoring at home with the Amsler grid in order to determine if there have been any changes in distortion.
Patients should go the clinic before the scheduled date in case there is a symptomatic decrease in vision or an increase of distortion.
In every examination, patient’s vision loss will be assessed, as well as any increase in image distortion. A macular OCT will also be performed in order to assess whether there has been progression in macular epiretinal membrane.

Contact us or request an appointment with our medical team.