Diabetic retinopathy is a vascular disease secondary to diabetes. Diabetes is a metabolic disease with a growing prevalence in our society that damages the small blood vessels of the retina due to the metabolic decompensation that it causes. The retina is a thin layer of light-sensitive tissue that lines the back of the eye. It is the element where light rays are focused to transmit them to the brain and interpret them as images. The damage causes a loss of vision that can be very considerable and irreversible.
The high levels of glycaemia in a sustained manner alter the walls of the small retinal vessels and make them more permeable and irregular. From these initial lesions, retinopathy can evolve in different stages.
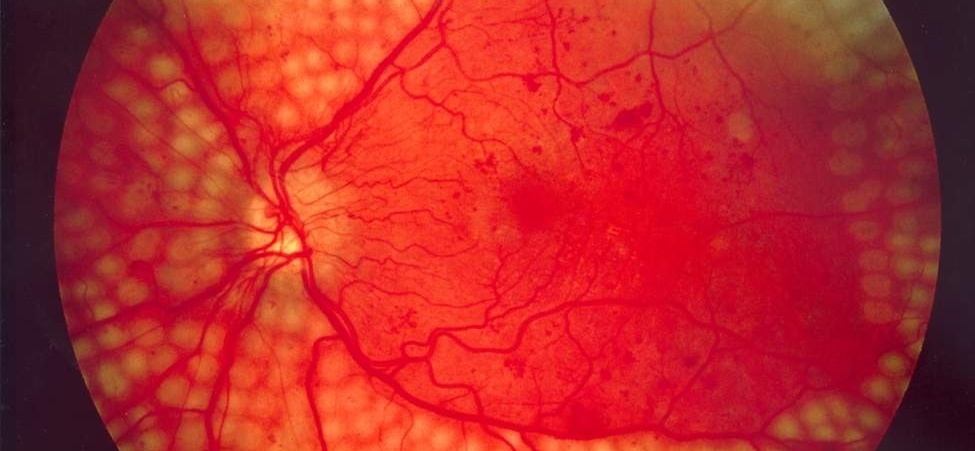
Depending on the type and extent of the typical signs of diabetic retinopathy (RD), such as microaneurysms, microhemorrhages, micro-infarcts, lipid exudates, neovessels, etc., the disease is classified into several stages: mild, moderate, severe and proliferative.
Diabetic macular oedema (DME) can occur in all forms of diabetic retinopathy, which is the main cause of decreased visual acuity in cases of diabetes.
Diabetic macular oedema is the accumulation of fluid in the macula, the central area and most sensitive of the retina, responsible for good visual acuity.
In the initial phase, diabetic retinopathy does not cause changes in vision, but as the stages progress, it can worsen and cause severe vision loss and even blindness.
The most frequent symptoms are the decrease in visual acuity, metamorphopsias (deformed vision of objects) and myodesopsias (spots that float in the field of vision, also known as floating flies,).
The fact that in the initial stages does not cause symptoms means that many times the patient is not aware that he has the disease until he is already in advanced stages. That is why it is so important that diabetics undergo screening.
People with diabetes, both type 1 and type 2, are at risk of suffering from it, so it is very important that they undergo a complete ophthalmological examination at least once a year. A large percentage of diabetics develop diabetic retinopathy in some of its phases.
The complications that usually arise due to diabetic retinopathy are vitreous hemorrhages, detachments of tractional retina and neovascular glaucoma, which usually require surgical treatment.
Diabetic retinopathy affects patients in different ways, depending on the degree of the disease and the affected area (macula or central area and periphery). Therefore, there are several treatments available.
Laser photocoagulation, both standard and subthreshold, creates small therapeutic burns on the retina. There are also intravitreal injections of drugs (antiangiogenic or corticoids) and vitrectomy, which is the vitreorretinal surgery indicated for vitreous hemorrhages or tractional detachment of the retina.
Apart from the specific treatment of the eye, strict metabolic control of diabetes is essential and very important in the evolution and prognosis of retinopathy, following the guidelines of medication, diet and physical exercise recommended by the diabetologist.
However, people who suffer an initial phase of diabetic retinopathy may not need treatment, although they will need detailed follow-up.

Contact us or request an appointment with our medical team.